For raw milk production, risk management and customer satisfaction go hand-in-hand. Many of the strategies that result in low-risk raw milk also work well to keep customers happy with delicious, long-lasting milk. Rapid chilling is one such strategy that lowers the risk of pathogens while also improving the flavor and shelf-life of raw milk.
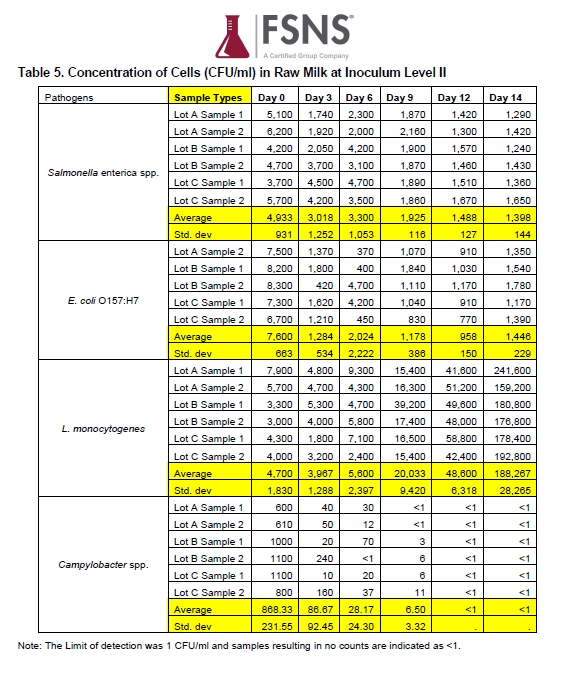
Although pathogens in well-produced raw milk are rare, they are still an important consideration and we encourage all raw milk farmers to take pathogens seriously. The four main pathogens of concern that can be found in raw milk are E coli 0157:H7, Salmonella spp., Campylobacter spp., and Listeria monocytogenes. Illnesses from these pathogens can be serious or even fatal.
In the rare case when pathogens are present in well-produced raw milk, illness will still not occur unless the pathogen load (or amount of pathogen present) is high enough to produce illness. If it is present in a small enough quantity, even the most virulent pathogen will not produce illness. Generally, the presence of a single virulent bacterium is not sufficient to cause illness, and different pathogens have varying thresholds at which they must be present to induce human illness.
However, bacteria multiply rapidly at warm temperatures and can double their count in as little as 20 minutes. At cold temperatures, bacteria growth slows down dramatically. This means that farmers can greatly reduce the number of bacteria present in raw milk by quickly chilling the milk right after milking time.
Aim for Chilling to 35-40 °F in Less Than an Hour
Our general recommendation is for farmers to chill their raw milk to 35-40 °F within an hour of milking. This helps in ensuring that any bacteria present in the raw milk do not have much time in which to multiply.
Refrigerators do not generally work well for rapidly chilling raw milk. Depending on the size of the milk jar or jug, it may take a few hours for warm milk to cool down to under 40 degrees in the refrigerator. Freezers also do not generally work well for chilling milk because the milk may freeze and break the glass jars.
In order to achieve cold milk in a short time, other methods are needed. We work closely with dozens of farmers, and have seen that rapid milk chilling is achievable no matter the size of the farm. Here are some of the different ways in which farmers can rapidly chill their raw milk to 35-40°F in an hour or less.
Ice-and-Water Bath for Rapid Milk Chilling on Micro-Dairies
For small-scale farms, an ice-and-water bath can work well for milk chilling. A chest cooler can be used to hold the ice-and-water bath. When using this method, there are a few important things to pay attention to:
The milk jars should be submerged in the cold ice-and-water, but make sure that the water level does not reach lid of the milk container. Otherwise, there may be problems with water comingling with the milk in the jars.
The size of the milk jar will make a big difference in how long it will take the milk to chill down. We recommend that farmers use milk jars that are no larger than ½ gallon, or else the chilling time will be too lengthy.
Some farmers who do not have ice maker machines have preferred to use either stainless steel ice cubes (which can be sanitized in the dishwasher) or frozen water bottles which can be reused over and over again.
Make sure there is enough cold ice water to rapidly chill the milk. If there are too many milk jugs in relation to the amount of ice water, then the chilling will not be quick enough.
Some farmers like to add in a small submersible water pump (such as an aquarium or pond pump) to circulate the water in their ice water bath for quicker chilling.
Whatever method you use, you can check to see whether the milk is chilling rapidly enough by measuring the temperature in the middle of your milk jars after an hour.
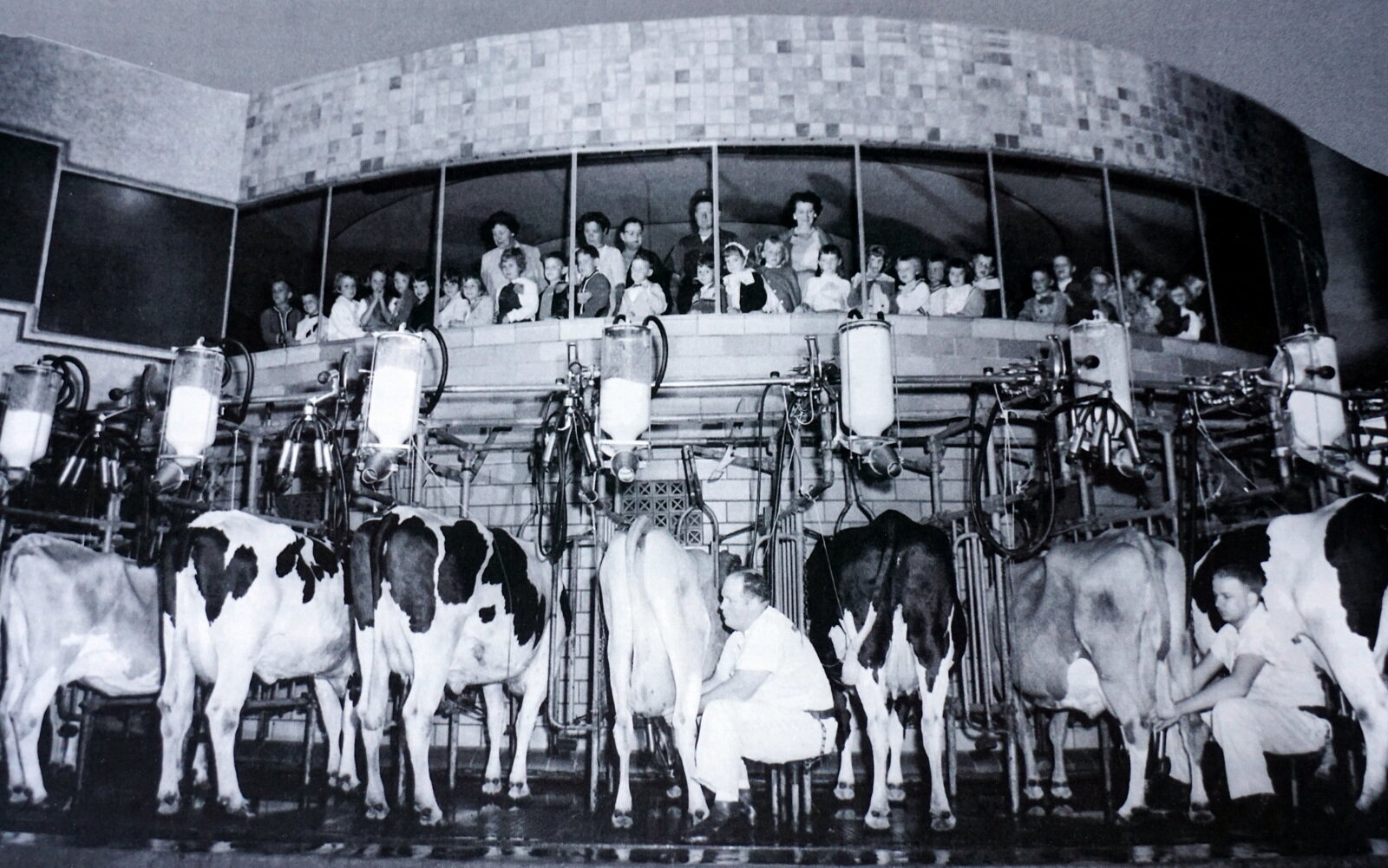
Bulk Milk Tanks
Bulk tanks are another option for milk chilling. Small bulk tanks can hold up to 15 gallons of milk, and many other sizes are available for farmers who are producing larger quantities of milk. Bulk tanks with integrated cooling systems can quickly chill the milk to the desired temperature. When using a bulk tank, farmers need to be aware of the following:
Bulk tanks need to be sized appropriately, or else there can be problems with the milk freezing if there is too little quantity of milk relative to the size of the tank.
Milk stacking occurs when milk from multiple milkings is poured into the bulk tank. This can result in increased bacteria counts as the milk in the tank is re-warmed each time fresh milk is added. Furthermore, milk stacking increases the risk of contamination from one batch of milk to another, thereby increasing the potential damage done by the presence of any undesirable bacteria/pathogens. We recommend that farmers minimize milk stacking by bottling their milk after every 1-3 milkings.
Bulk tanks must be thoroughly cleaned after each time the milk is bottled. The valve on the bulk tank, in particular, needs to be completely disassembled and scrubbed clean to ensure that it does not harbor bacteria.
Sophisticated Chilling for Larger Farms
Larger farms may choose to use sophisticated chilling equipment, such as plate chillers. These chillers will cool the milk down rapidly in just a few minutes before it even enters the bulk tank. Farmers using plate chillers need to be aware of the following:
Complex equipment can create more opportunities for bacteria biofilms to grow in nooks and crannies. Therefore, thorough cleaning is essential for plate chillers in between milkings.
A clean-in-place (CIP) system will be required for thoroughly cleaning the plate chiller. We recommend that farmers work with a dairy supply consultant to optimize the CIP for their individual pipeline systems. This should include a tepid rinse, followed by a hot wash with alkaline detergent, followed by a warm acid rinse.
The temperature of the water used for the hot alkaline wash will decrease as the water flows through the system, thereby reducing the effectiveness of the cleaning solution. It is recommended to ensure that the temperature of the wash water is at least 120 degrees at the outlet of the system.
Over time, bacteria biofilms can become resistant to specific cleaners, especially in pipeline systems. Therefore, it is recommended to periodically “shock” pipeline systems by using different alkaline and acid cleaners about once a month.
Rapid Milk Chilling is Achievable
Rapid milk chilling is an important strategy for risk reduction with raw milk. As we have described, rapid chilling is achievable no matter the size of the farm. Besides reducing the risk of high bacteria counts in the milk, rapid chilling can also result in a longer shelf-life for the milk and help in preventing off flavors. Rapid chilling is a Win-Win for both farmers and customers.
This article was published in the April 2023 issue of Graze Magazine.