Ongoing bacterial testing is a crucial part of raw milk risk management.
Consumer demand for raw milk is increasing, as people learn about the health benefits of raw milk and the negative effects of pasteurization. Raw milk farmers can thrive in this burgeoning market and help their customers achieve robust health with strong immune systems and resistance to asthma and allergies.
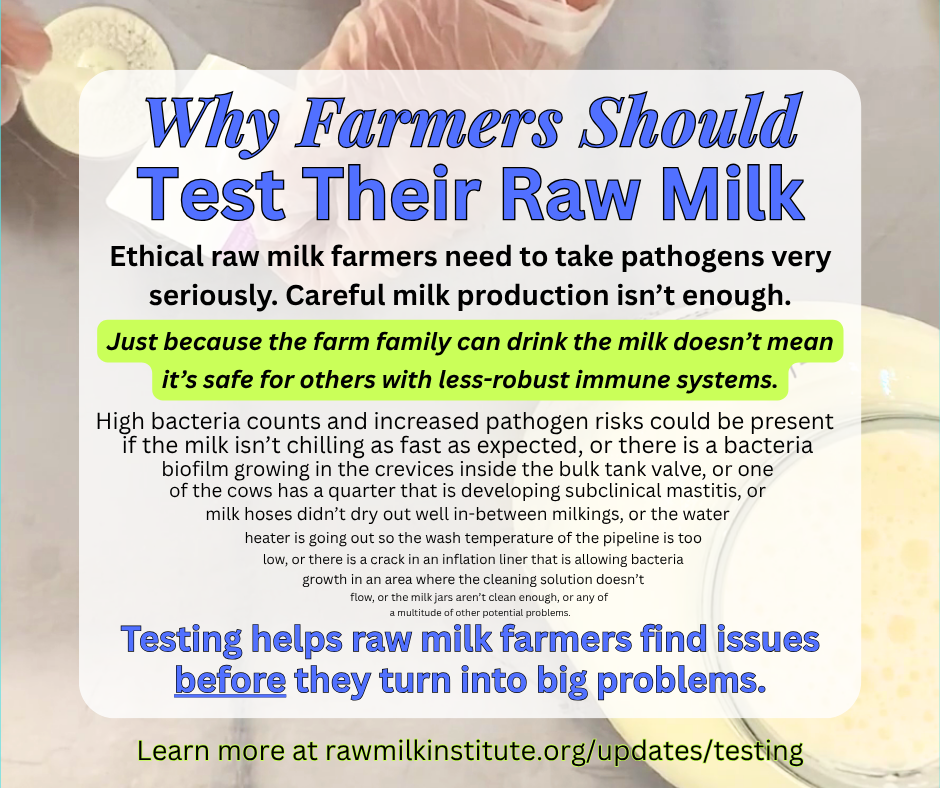
Unfortunately, that service to humanity can be overshadowed if farmers aren’t diligent about managing the real food safety risks that accompany raw milk. Some people and organizations have asserted that raw milk is inherently safe because of the natural bacteria that is present. However, this is demonstrably not true. Pathogens can indeed be present in raw milk and those pathogens can make people sick. Ethical farmers need to take these risks seriously and work actively to mitigate them.
Scroll or click below for information about the following topics:
Top 4 Pathogens of Concern for Raw Milk
The four most common human pathogens that have been associated with raw milk-related illness are verotoxin producing Escherichia coli (VTEC, such as E. coli O157:H7), Salmonella enterica spp., Campylobacter jejuni, and Listeria monocytogenes. When any of these bacteria are present in the milk at levels that are sufficient to cause infection, susceptible people may experience intestinal illness that may include severe illness or death.
E. coli 0157:H7 is of particular concern because it can produce severe illness even with a low pathogenic load. With even just a few bacteria present, E. coli O157:H7 can lead to hemolytic uremic syndrome (leading to kidney failure) or thrombocytopenic purpura (blood clots that can restrict flow of oxygen to the organs).
Thus, pathogens in raw milk need to be taken very seriously by farmers. Some of the most common sources of pathogens in milk are manure, mastitis, and improper cleaning of milking equipment resulting in biofilms of bacteria.
"But My Family Drinks My Milk with No Problems"
Farmers, please don’t make the mistake of assuming that, just because your family can drink your raw milk with no problems, there are no pathogens present.
We commonly hear farmers say they would know if there was a problem with their milk, because their own family drinks it without issues. However, this is not necessarily true. Farm families generally have more-robust immune systems than the population at large. Being around animals and the farm environment tends to build strong immune systems, but many raw milk customers have no such advantages.
Some people choose to drink raw milk specifically to help build up their immune systems. As such, they may have leaky gut, compromised immune systems, improper gut flora due to antibiotics, extreme vulnerability while recovering from chemotherapy, etc. These customers will have a much lower threshold for illness from pathogens than farm families. Just because the farm family can drink the milk with no issues does not mean that the raw milk consumers will be able to do so.
Careful Milk Production Isn't Enough
Important risk management strategies for low-risk raw milk include careful udder preparation, rapid milk chilling, thorough equipment cleaning, and much more. Our experience in mentoring hundreds of farmers has shown that these careful practices aren’t enough, though. They must be backed up with bacterial testing to ensure that nothing important is being missed.
We’ve seen it happen time and time again that farmers can get an unpleasant surprise when they first test their milk. Low-risk raw milk requires careful attention to a multitude of details, and even one little missed detail can turn into a big problem. Bacterial testing serves as a confirmation step to make sure the overall milk production process is working well to reduce the risks.
Farmers: if you don’t test your milk, you won’t know. As Raw Milk Institute Chairman Mark McAfee says, “What gets tested gets done.” It could be that:
the milk isn’t chilling as fast as expected, or
there is a bacteria biofilm growing in the crevices inside the bulk tank valve, or
one of the cows has a quarter that is developing subclinical mastitis, or
the milk hoses didn’t dry out well in-between milkings, or
the water heater is going out so the wash temperature of the pipeline is too low, or
there is a crack in an inflation liner that is allowing bacteria growth in an area where the cleaning solution doesn’t flow, or
the milk jars aren’t clean enough, or
any of a multitude of other potential problems.
All of these can lead to increased bacteria counts, so testing is a way to double-check that nothing important has been missed.
Which Tests to Perform
Pathogen testing of raw milk can be used to determine whether specific pathogens are present by testing for Escherichia coli VTEC, Salmonella enterica spp., Campylobacter jejuni, and Listeria monocytogenes. Pathogen testing can have both false positives and false negatives, so it is not a perfect guarantee of food safety. Additionally, pathogen testing can be cost-prohibitive and is only meaningful if it is performed frequently. Nonetheless, for farmers who can afford it, frequent pathogen testing can be helpful in determining whether any specific pathogens are present over time.
Regardless of whether or not pathogen testing is performed, Raw Milk Institute (RAWMI) recommends that all raw milk farms perform bacterial testing at least monthly for coliforms and Standard Plate Count (SPC). The RAWMI Common Standards aim for a rolling three-month average of:
<5,000 cfu/mL for SPC
<10 cfu/mL for coliforms
Although these two tests do not directly detect the presence of pathogens, they serve as general indicators that the milk is being produced hygienically and in such a way that pathogens are less likely to be present.
NOTE: None of these tests are a perfect guarantee that there will never be a pathogen present. No food can ever be perfectly safe. Nonetheless, these tests can help dramatically decrease the risk of having pathogens present.
Where to Test Raw Milk
Depending on location, milk testing may be performed at a local university or independent testing lab. Additionally, some labs have created specialized testing packages for raw milk.
Microbial Research lab in Fort Collins Colorado has a raw milk testing package that makes it more affordable for farmers to perform pathogen tests. The standard tests which are included are Coliforms, Standard Plate Count, Salmonella, and E. coli O157. Other tests such as Campylobacter and Listeria are also available. Additionally, there is a raw milk shipping kit available.
MB Labs in British Columbia Canada has a testing package for raw milk. The test package includes Total Coliforms, Standard Plate Count, Fecal Coliforms, E. coli, Campylobacter, Listeria (Total & L. monocytogenes), Salmonella, and Shigella.
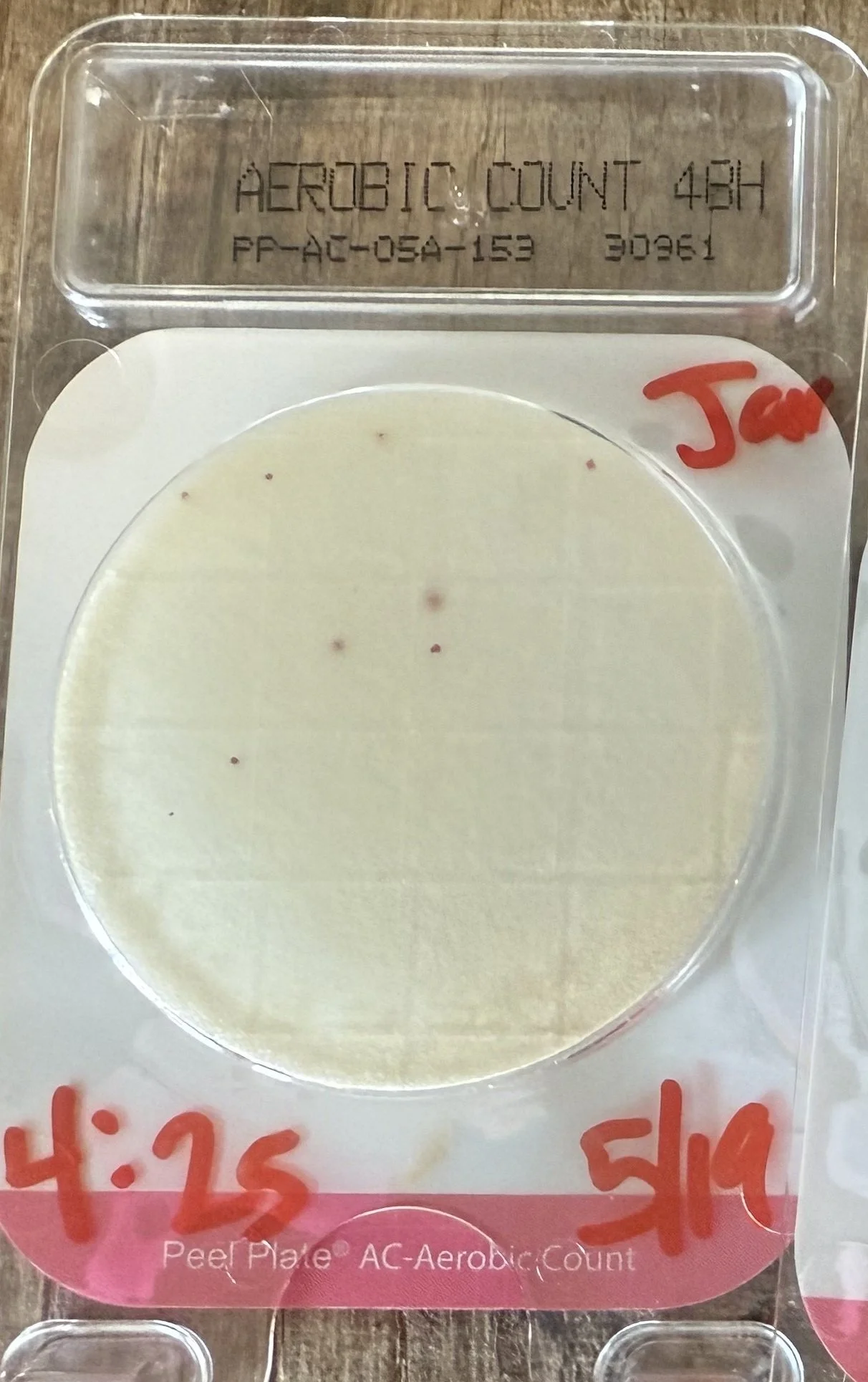
On-farm labs are a good option for many raw milk farmers. After an initial investment in equipment, on-farm labs can greatly reduce testing costs in the long-term because the testing cost is only $1-3 per test.
On-farm labs can be used for coliform and Standard Plate Count testing, with results in 24-48 hours.
On-farm labs make it easy and economical to test milk such that farmers can test more often, such as weekly or even daily. Testing more frequently allows farmers to identify and troubleshoot any problems much more quickly.
We have a comprehensive guide to on-farm testing here.
Raw Milk Institute does not generally recommend on-farm testing for specific pathogens (such as E coli 0157:H7, salmonella, listeria mono, etc), due to potential hazards from accidental release of pathogens on the farm. However, specialized test systems are being developed for on-farm testing of pathogens. In those systems, the test samples are destroyed after each test. Those test systems are stand-alone and may be cost-prohibitive for some farmers. Nonetheless, these test systems may be a good option for farmers who want to perform more frequent pathogen testing.
Spectacular Labs has developed a stand-alone pathogen test system with results in 6-12 hours (depending on which pathogen is being detected).
The Spectacular Labs system is self-contained and destroys the sample once the test is completed (thereby eliminating the risk of pathogen escape).
Testing is a Proven Part of Low-Risk Raw Milk
It is important to note that there is no such thing as a perfectly safe food. A CDC analysis of foodborne illnesses from 2009-2015 showed that the top food categories commonly linked to illnesses were chicken, pork, and seeded vegetables. Multi-state foodborne illness outbreaks have been linked to foods ranging from unpasteurized apple juice to ground beef to soy nut butter to lettuce. Pasteurized milk is not perfectly safe, either, and is implicated in foodborne illnesses and outbreaks every year.
The three pillars of the RAWMI Method for safe, low-risk raw milk are 1) farmer training, 2) risk management plan for each farm, and 3) bacterial testing of raw milk at least monthly for coliforms and Standard Plate Count per the Common Standards. Although there is no way to guarantee perfectly safe food, the RAWMI Method dramatically reduces the risk of illness from consumption of raw milk.
Researchers from Canada and Europe have studied the safety of raw milk intended for direct human consumption. They found that raw milk can be a low-risk food when farmers are trained in risk management practices, implement careful production practices, and test their milk regularly. Researchers concluded that “raw milk can be produced with a high level of hygiene and safety.” The evidence is clear that raw milk can be a low-risk food and ongoing milk testing is an important part of the overall risk management strategy.
Raw milk farmers have an ethical responsibility to take pathogens and food safety risks seriously. The production of safe raw milk is a long-term mission, never fully completed or fully perfected. There will always be something to learn and much to teach. Farmers can engage in our free mentoring program here: https://www.rawmilkinstitute.org/how-to-become-rawmi-listed
Disclaimer: The Raw Milk Institute provides information for educational purposes only. Raw Milk Institute does not assume any responsibility or liability for the use of this information.