Raw milk has long been at the center of passionate debate, with public health concerns often clashing against emerging research on its microbial complexity and potential benefits. A recent American Council on Science and Health (ACSH) commentary appears to overlook a growing body of peer-reviewed evidence. This review highlights key scientific advances that challenge outdated assumptions and call for a more balanced, evidence-based conversation.
This article is reprinted with permission from the ACSH. The original article is here.
Thank you to the American Council on Science and Health (ACSH) for the opportunity to present a body of scientific evidence available in peer-reviewed studies that Dr. Billauer appeared unaware of in her post about raw (unpasteurized) milk. Our concern is that the November post is at odds with the growing corpus of scientific evidence from the peer-reviewed literature. Here are six claims unsupported by the current body of evidence, each with a brief bulleted description of the evidence and a hyperlinked citation. A more comprehensive documentation can be found here.
1. Dr. Billauer claimed that percentages of raw milk outbreaks compared to all outbreaks associated with food and water had decreased from ~25% in 1938 to ~1% in 2005, but that ‘of late’, ‘the figure has blossomed’.
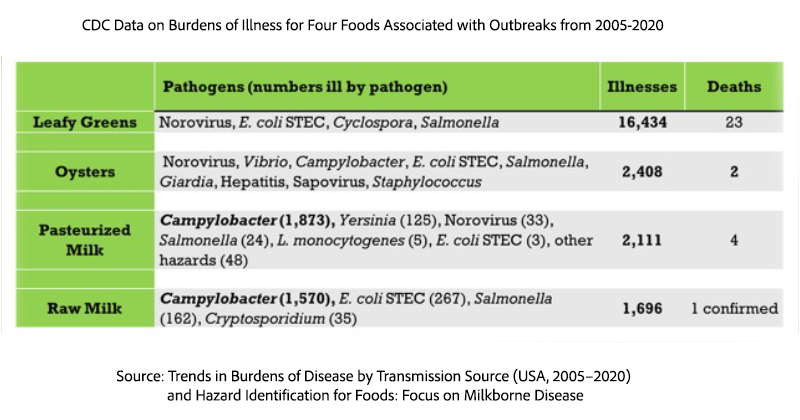
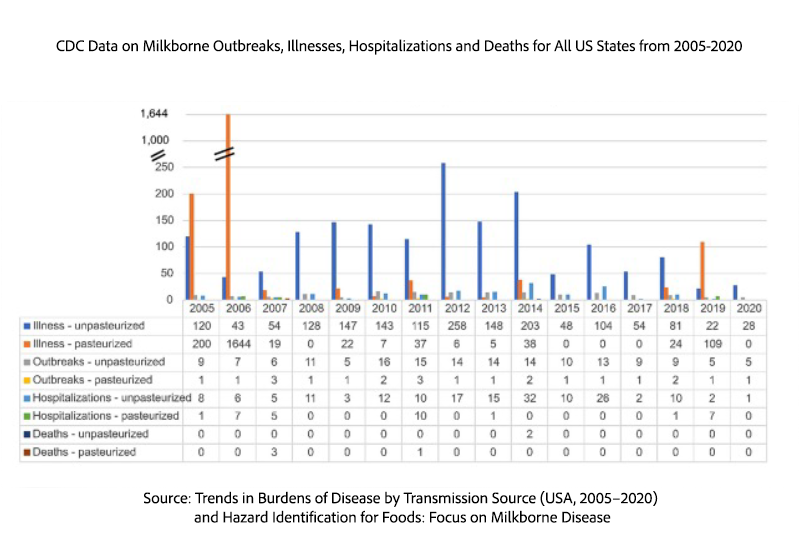
Raw milk outbreaks and illnesses as a percentage of foodborne and waterborne outbreaks and illnesses have not increased from 2005-2020 (Stephenson et al., 2024).
1% of outbreaks associated with food and water for this period (162/15,430) were attributed to raw milk.
0.6% of illnesses associated with food and water for this period (1,696/304,491) were attributed to raw milk.
2. The November post claimed that the ‘predominant diseases associated with raw milk consumption today are Salmonella, Listeriosis, and avian influenza H5N1’ associated with ‘escalating [raw milk] outbreaks throughout the country’. No references were cited.
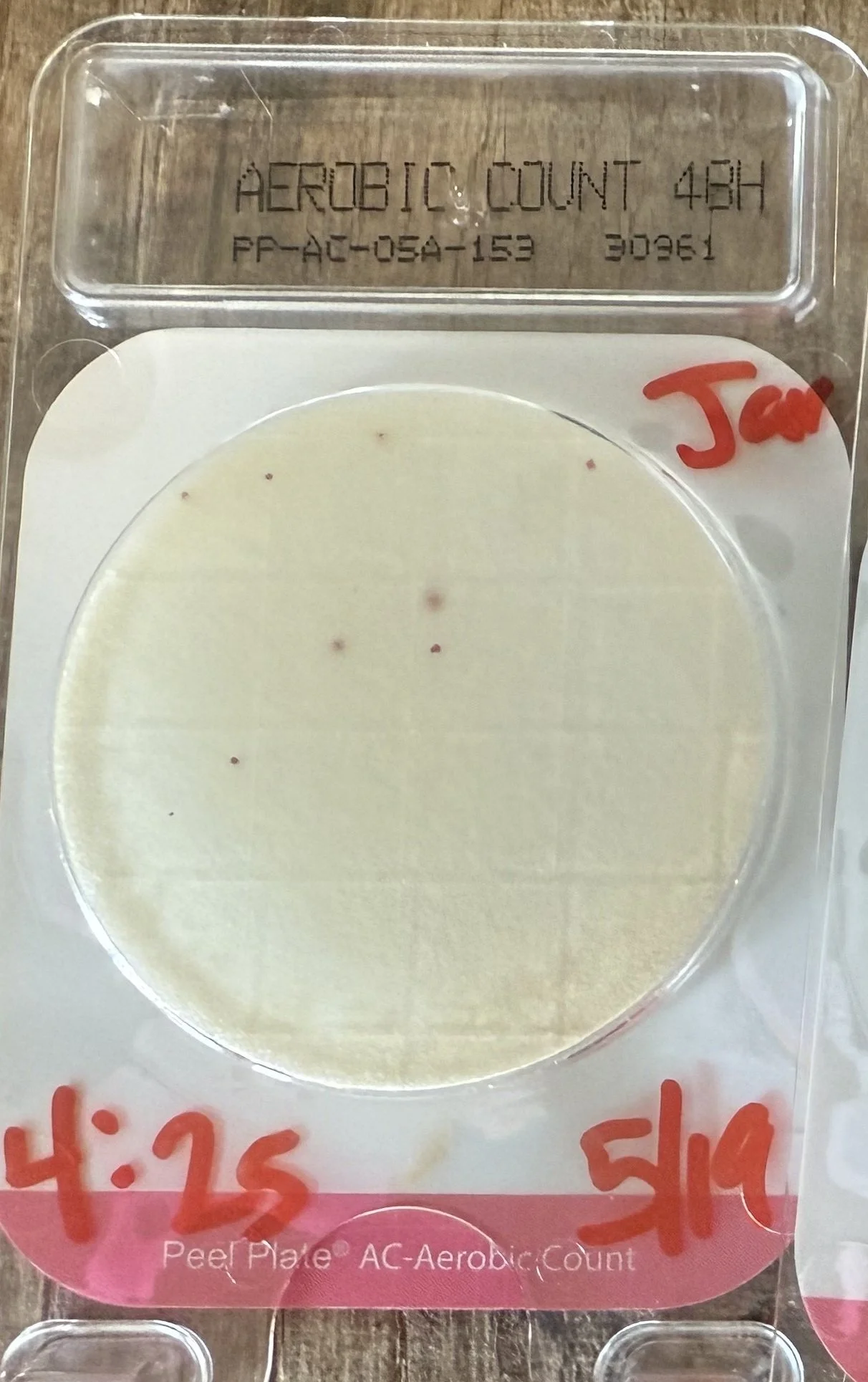
The 2024 epidemiologic study (Stephenson et al., 2024) documents: campylobacteriosis accounting for 1,570 illnesses, >90% of raw milk illnesses from 2005-2020 (see Table 1 below); 162 cases of salmonellosis associated with raw milk of the total 22,943 cases; no confirmed cases of listeriosis associated with raw milk (though 5 cases associated with pasteurized milk).
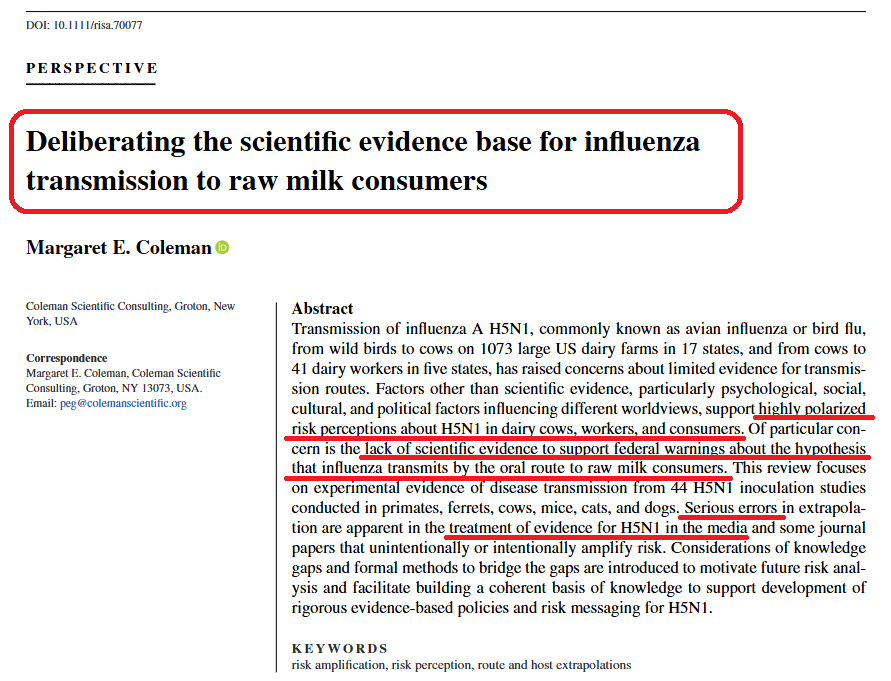
No evidence supports the claim that influenza H5N1 caused illness among raw milk consumers (see Coleman, 2025) based on the framework for assessing influenza transmission Killingley and Nguyen-Van-Tam, 2013). Although oral transmission of H5N1 in humans has been simulated based on ‘what-if’ extrapolations at three levels of evidence (Chen et al., 2025), no epidemiologic or experimental evidence for oral disease transmission exists for H5N1 in primates, including humans.
A recent outbreak study (Weinstein et al., 2025) reported 9 initial cases of salmonellosis associated with raw milk in California in October of 2023. A Salmonella Typhimurium sequence isolated from raw milk was retrospectively matched to strains from 145 other clinical cases in 5 states between September 2023 and March 2024, identified through the national network of public health laboratory databases, PulseNet. No deaths and 22 hospitalizations were associated with this outbreak. Some of the cases reported consuming raw milk.
Regarding the claim of an escalating number of raw milk outbreaks nationwide, no increasing trend was documented in numbers or rates (Figure 13 from Stephenson et al., 2024) of milkborne outbreaks, illnesses, hospitalizations, or deaths involving raw milk in the US or any state. The lack of increasing trends was consistent over multiple studies using established epidemiologic methods of analysis (Whitehead and Lake, 2018; Koski et al., 2022; Stephenson et al., 2024).
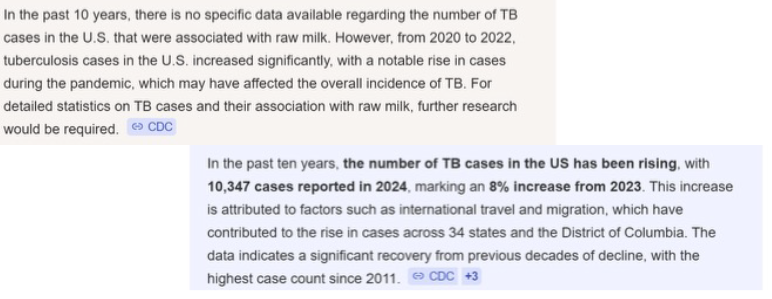
3. The November post claimed that ‘The White Plague’ (tuberculosis or TB) ‘Returns’ with increasing access to raw milk.
No evidence links Mycobacterium bovis to human TB cases in the US in recent years, a statement supported by peer-reviewed studies cited in our comprehensive document and the following relevant AI summaries.
4. The November post cited an outdated reference from 2015 claiming no evidence of benefits for raw milk consumption and further claimed that ‘This has not changed [since 2015],’ without any reference.
Thirteen peer-reviewed studies provide clinical evidence on the benefits and risks of raw and pasteurized milks, which merit deliberation by ACSH readers. The studies in bold are US cohorts.
Study Authors and Titles
Loss et al., 2015 - Consumption of unprocessed cow's milk protects infants from common respiratory infections
Brick et al., 2016 - ω-3 fatty acids contribute to the asthma-protective effect of unprocessed cow's milk
House et al., 2017 - Early-life farm exposures and adult asthma and atopy in the Agricultural Lung Health Study
Schröder et al., 2017 - A switch in regulatory T cells through farm exposure during immune maturation in childhood
Muller-Rompa et al., 2018 - An approach to the asthma-protective farm effect by geocoding: Good farms and better farms
Wyss et al., 2018 - Early-life farm exposures and eczema among adults in the Agricultural Lung Health Study
Abbring et al., 2019 - Milk processing increases the allergenicity of cow's milk—preclinical evidence supported by a human proof-of-concept provocation pilot
Sozanska, 2019 - Raw cow's milk and its protective effect on allergies and asthma
Brick et al., 2020 - The beneficial effect of farm milk consumption on asthma, allergies, and infections: from meta-analysis of evidence to clinical trial
Butler et al., 2020 - Recipe for a healthy gut: Intake of unpasteurised milk is associated with increased Lactobacillus abundance in the human gut microbiome
Järvinen et al., 2022 - Biomarkers of development of immunity and allergic diseases in farming and non-farming lifestyle infants: design, methods, and 1-year outcomes in the “Zooming in to Old Order Mennonites” Birth Cohort Study
Wyss et al., 2022 - Early-life farm exposures and eczema among adults in the Agricultural Lung Health Study
Pechlivanis et al., 2023 - Continuous rather than solely early farm exposure protects from hay fever development
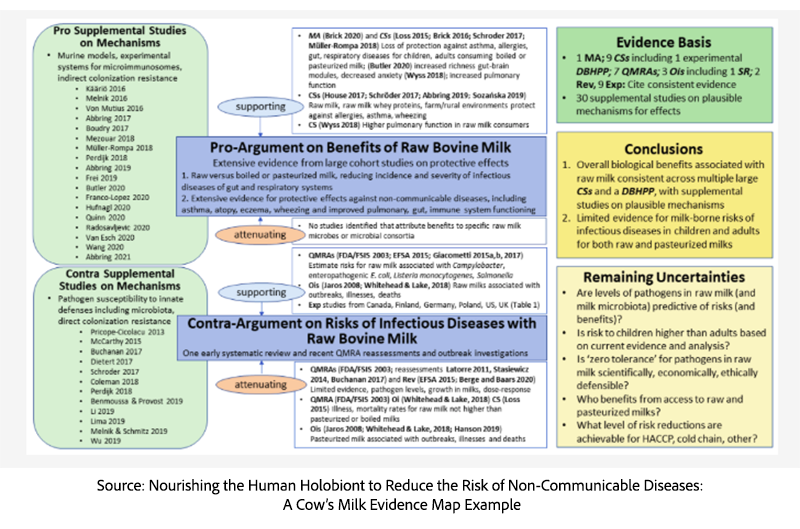
Also relevant is an evidence map analysis on the benefits and risks of raw and pasteurized milks. This study incorporated evidence from the first 10 studies and mechanistic studies that illuminate the underlying processes and pathways linking the natural milk microbiota to gastrointestinal, respiratory, neural, and immunological systems.
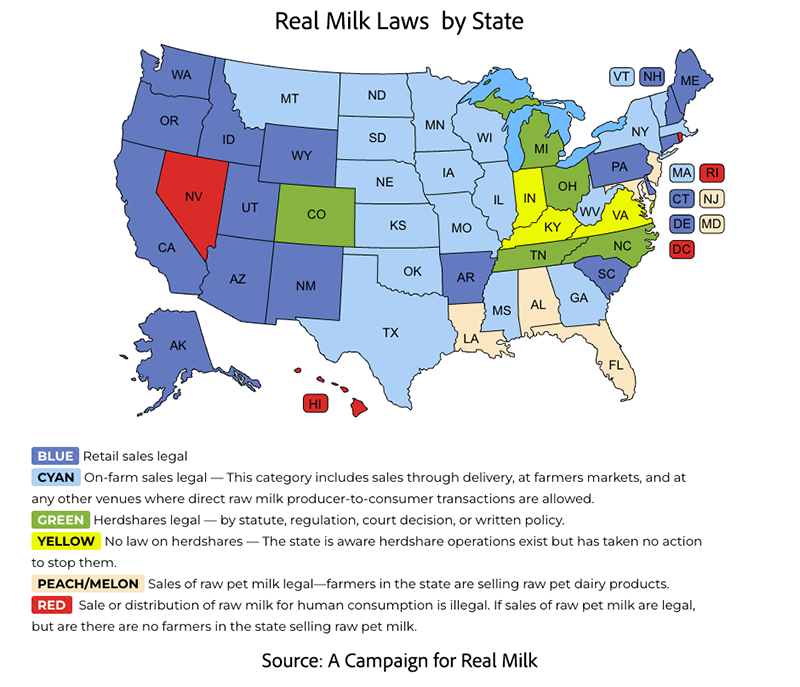
5. Dr. Billauer’s post claimed that ‘some 20 states explicitly prohibit access’ to raw milk; state rights (allowing constituents seeking raw milk the freedom to purchase it legally) versus ‘wrongs’ (‘likely responsible for the deaths of others’).
This claim is inaccurate and misleading. Thirty-four states permit either retail or on-farm sales to consumers, according to the map (last updated in September 2025).
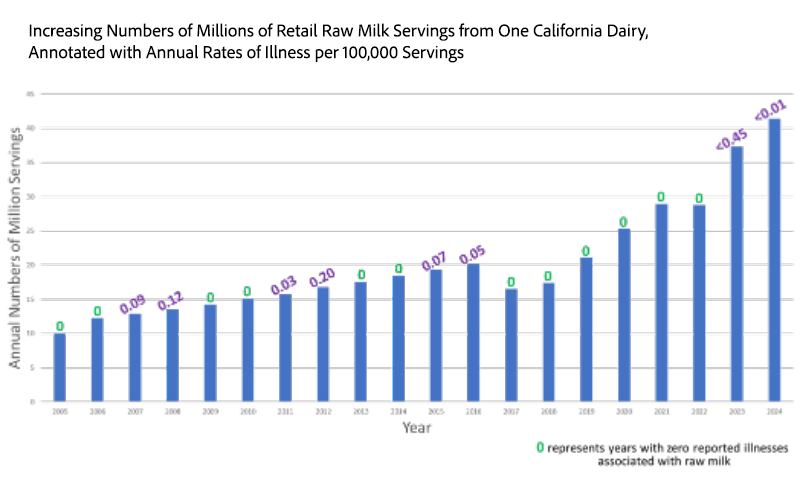
Further evidence of the safety record of raw milk included consideration of limited data on raw milk production as a surrogate for consumption. Retail production data for a large California dairy (Raw Farm, personal communication, Aaron McAfee) are reported in millions of annual servings for 2005-2024, with annotations for estimated annual illness rates per 100,000 servings from the CDC. Over the past 20 years in California, there have been no deaths, and annual illness rates have been <0.45 per 100,000 servings, despite increasing production. For 12 of the past 20 years, no reported illness was associated with raw milk consumption in California.
The Stephenson study reports that increasing legal access was not associated with increased illness, based on statistical comparisons across 7 states with data available before and after the increase. Additionally, over the period 2005-2020, a single death associated with raw milk was confirmed in an adult with underlying chronic illness. Death is thus unlikely, according to epidemiologic evidence.
6. The November post cited a series of essays and speeches by businessman and philanthropist Nathan Strauss, compiled by his wife, Lina Gutherz Strauss, and published in book form between 1913 and 1917.
This afforded ACSH readers an incomplete perspective at best, dominated by outdated opinions that do not reflect a comprehensive, coherent, and transparent body of evidence that includes knowledge of the milk microbiota and other 21st-century scientific advances.
The post’s ‘Short History’ overemphasized the portion of history that reflected Mr. Straus's ‘crusade to promote pasteurization’. Excluded is a rich history from the 1850s onward, documented in the peer-reviewed literature on adulterated ‘swill milk’ from sick cows confined in urban environments versus Certified Raw Milk from healthy pastured cows overseen by medical professionals. [1]
To address this excluded portion of history, we note the following references:
The Human Superorganism: How the Microbiome is Revolutionizing the Pursuit of a Healthy Life provides context on our microbiota as our partners in health and the importance of ‘seeding and feeding’ the gut microbiota to reverse the current epidemic of noncommunicable diseases in the US
Blind Spots: When Medicine Gets It Wrong, and What It Means for Our Health: Dr. Markary cautions that his fellow physicians and their institutions created and maintain ‘blind spots’, unquestioningly believing entrenched dogma and defending it by suppressing or excluding emerging scientific evidence for many decades
The Germ in the Dairy Pail: The 200-year War on the World’s Most Amazing Food-Milk: meticulous research identified extensive evidence from medical, social, industrial, and agricultural drivers that prioritized economic and political interests over public and animal health; provided quotations from physicians, veterinarians, scientists, and businessmen including John D. Rockefeller and author and investigative journalist Upton Sinclair (The Jungle) that have been largely ignored or suppressed for nearly a hundred years.
“Certification of milk by medical commissions [Certified Milk Program] offers the best solution to our milk problem. Not through heat, which destroys vital elements, but through cleanliness and careful monitoring” - Dr. Henry Coit, founder of the Certified Milk Program, 1893
Taken together, the scientific evidence presented here reveals that the risks and benefits of raw and pasteurized milk are far more nuanced than portrayed in the November post. Contemporary epidemiologic studies show no national trend of increasing raw milk outbreaks, while a substantial and growing literature documents potential protective effects linked to the natural milk microbiota—particularly for immune and allergic disease outcomes. By relying on outdated historical narratives and incomplete references, the post misses critical 21st-century advances in microbiology, risk analysis, and food science. A truly informed public health dialogue must move beyond entrenched dogma and engage transparently with the full scope of current peer-reviewed evidence. We welcome comments, particularly with links to additional evidence for further deliberation. A bibliography for 50 references cited in the comprehensive documentation of this work is also provided for interested readers who prefer this format to the hypertext-linked references provided herein.
D. Warner North is a decision science scholar and risk analysis consultant with over 50 years of experience. He served as President of the Society for Risk Analysis (SRA) and as area editor for decision analysis for the SRA journal Risk Analysis. Dr. North has received several awards recognizing his extraordinary leadership and achievements in both SRA and the Decision Analysis Society.
Margaret E. (Peg) Coleman is a medical microbiologist and consultant in microbial risk analysis with over 30 years of experience. Ms. Coleman served on the editorial board of the Society for Risk Analysis (SRA) journal Risk Analysis. She was selected as an SRA Fellow in 2020 and elected to the SRA Council (2022-2024). Ms. Coleman serves as an unpaid advisor to the Raw Milk Institute and the Canadian Artisan Dairy Alliance.